Spinal compression fractures occur when the vertebrae in the spine collapse or break due to weakened bones, often seen in conditions like osteoporosis. This can result in significant pain and limited mobility for individuals affected, but CFRS is here to help.
Compression Fracture Q & A
What is a compression fracture?
What symptoms does a compression fracture cause?
What treatments are available for a compression fracture?
What is a compression fracture?
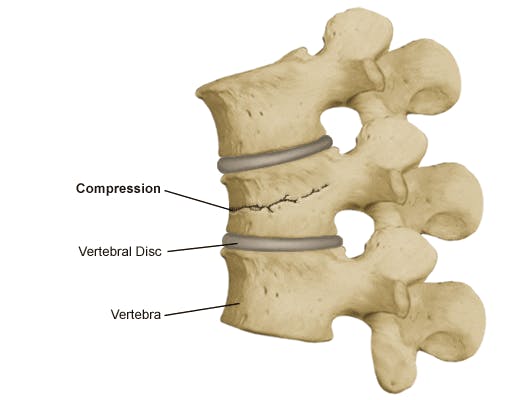
A compression fracture occurs when a bone breaks because it's not strong enough to support the weight it usually carries. Rather than snapping or shattering, the bone flattens and compresses. Vertebral compression fractures are the most common type. Vertebral compression fractures are sometimes due to traumatic injuries like falls or auto accidents. Tumors in or on your spine can also make the bone so weak it collapses. The leading cause of vertebral compression fractures, however, is osteoporosis. Osteoporosis is a condition where your bones lose their density, making them weak and brittle. If you have advanced osteoporosis, your bones can fracture easily, even when you're doing everyday activities, and vertebrae are especially vulnerable.
What symptoms does a compression fracture cause?
The main symptoms of a vertebral compression fracture are pain and spinal deformity. When the fracture occurs, you might have back and neck pain that worsens if you cough or sneeze. When you have one vertebral compression fracture, others are likely to follow, compounding your pain. If you've got several vertebral compression fractures, you might have a hunched appearance in your upper back. This condition, known as kyphosis, develops because most vertebral compression fractures affect the front of the bone, so the vertebra becomes wedge-shaped. A series of wedge-shaped vertebrae creates a curvature at the top of your back that's known as a dowager's hump.
What treatments are available for a compression fracture?
To address the immediate pain and disability, the team at Center for the Functional Restoration of the Spine can perform either:
Vertebroplasty
Minimally invasive vertebroplasty is a procedure in which your provider injects a special medical cement into the compression fracture using imaging technology to guide the needle. The glue strengthens and stabilizes the vertebra, reducing your back pain.
Kyphoplasty
Kyphoplasty uses a similar technique to vertebroplasty but has an extra stage. Before injecting the bone cement, your provider inflates a tiny balloon inside the affected vertebra that raises the bone to a more normal height. Kyphoplasty can help reduce the severity of your kyphosis to stabilize your spine and lessen back pain. In addition to treating your vertebral compression fracture, it's important to take steps to slow osteoporosis progression if that's the reason for your condition. This may mean taking bisphosphonates and monoclonal antibody medications to strengthen your vertebrae and reduce the risk of further compression fractures.
If you're experiencing back pain or developing a dowager's hump, call Center for the Functional Restoration of the Spine today to schedule a consultation or book an appointment online.